In the realm of healthcare, billing can be a complex and frustrating journey, especially when it comes to claim denials. Did you know that nearly 1 in 5 claims are initially denied? That's a staggering statistic that highlights the importance of knowing how to navigate the appeal process. Understanding this process not only helps you recover lost revenue but also improves your overall Medical Billing Services efficiency. So, let’s roll up our sleeves and get to work!
What is a Denied Claim?
A denied claim is a request for payment from a health insurer that has been rejected for a specific reason. Common reasons for denial include:
- Incorrect information: This can be anything from a misspelled patient name to incorrect insurance details.
- Lack of medical necessity: Sometimes, insurers deny claims if they determine that the treatment wasn’t necessary.
- Expired coverage: If a patient’s insurance has lapsed, claims may be denied.
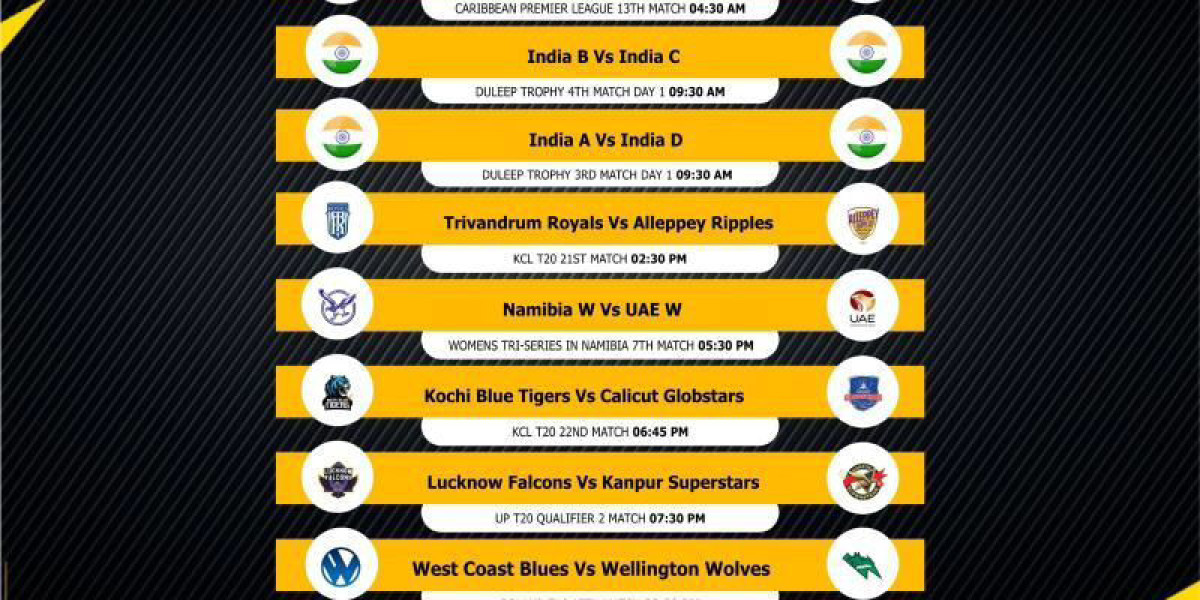
Types of Claim Denials
There are two main types of claim denials:
- Hard Denials: These cannot be appealed and often require you to re-submit with correct information.
- Soft Denials: These can be appealed and typically occur due to missing information or clarification needed.
Initial Steps After a Denial
When you receive a denial notice, take a deep breath—this is where your action steps begin.
Review the Denial Notice
Your first step should be to carefully review the denial notice. This document will outline the reason for the denial, which is crucial for understanding your next steps.
Gather Necessary Documentation
Collect all relevant documents, such as patient records, the original claim submitted, and any correspondence related to the claim. This will help you build a strong case for your appeal.
Understanding the Denial Code
Explanation of Denial Codes
Insurance companies use denial codes to communicate the reasons behind a claim denial. These codes can often seem like a foreign language, but understanding them is key to crafting an effective appeal.
How to Interpret These Codes
Take time to research what each code means Medical Billing and Coding Services. Many insurers provide a code lookup tool on their websites, which can be invaluable when you’re trying to decode the message behind the denial.
Researching Payer Policies
Before diving into your appeal, familiarize yourself with the specific payer’s policies related to the denied claim.
Importance of Knowing the Payer's Guidelines
Each insurance company has its own set of guidelines and requirements for claims. Knowing these can make or break your appeal.
Resources for Policy Information
Many payers have manuals or guidelines available online. Use these resources to ensure you’re aligning your appeal with their policies.
Preparing Your Appeal
Drafting an Appeal Letter
Now that you have all your information, it’s time to draft your appeal letter. This letter should be concise and clearly state your reasons for disputing the denial.
Key Components to Include in Your Appeal
- Patient Information: Full name, date of birth, and insurance information.
- Claim Information: Date of service, claim number, and relevant codes.
- Argument: A clear explanation of why you believe the claim should be paid, supported by documentation.
Submitting the Appeal
How to Submit Your Appeal Correctly
Ensure that you submit your appeal according to the payer’s specified guidelines. This may include submitting via mail or electronically Medical Billing Services In California.
Importance of Following Up
After submitting your appeal, mark your calendar for a follow-up. Many payers have specific time frames for reviewing appeals, so knowing when to check back is crucial.
Tracking Your Appeal Status
Methods for Tracking the Status of Your Appeal
Utilize online portals, if available, to track your appeal. You can also call the payer’s customer service for updates.
Keeping Records of Communication
Document every interaction you have regarding the appeal. This not only helps you keep track of progress but can also serve as a reference if further action is needed.
Understanding the Outcome
Once your appeal is reviewed, you’ll receive a notification regarding the outcome.
Possible Outcomes of an Appeal
- Approved: Your claim is paid.
- Denied Again: You may need to decide whether to appeal further.
- Partial Payment: You may receive a partial payment, with a reason provided.
Next Steps for a Denied Appeal
If your appeal is denied again, consider gathering more evidence or consulting with a billing expert for assistance.
Avoiding Future Denials
Tips for Preventing Claim Denials
- Verify Patient Information: Always double-check the accuracy of the information before submitting a claim.
- Document Everything: Maintain thorough documentation of all patient interactions and services rendered.
- Stay Updated: Keep abreast of changes in payer policies and coding guidelines.
Importance of Thorough Documentation
Strong documentation is your best defense against claim denials. It ensures that you have all necessary information at your fingertips when submitting a claim or appeal.
When to Seek Professional Help
Signs It’s Time to Consult a Billing Expert
If you find yourself facing frequent denials or if the appeal process becomes overwhelming, it may be time to seek professional help.
Benefits of Hiring a Professional
Billing experts can provide guidance and expertise that can significantly improve your appeal success rates, allowing you to focus on patient care instead.
Conclusion
Appealing a denied claim in healthcare medical billing may seem daunting, but with the right knowledge and preparation, you can navigate the process successfully. By understanding the denial codes, researching payer policies, and preparing a thorough appeal, you increase your chances of recovering denied claims. Remember, staying proactive and keeping meticulous records can go a long way in avoiding future denials.
Contact P3 Healthcare Solutions today to learn more about how our medical billing services can help your practice succeed. Call us at: Tel:8445573227. Visit us at our address: 3200 E Guasti Rd Suite 100, Ontario, CA 91761, United States.