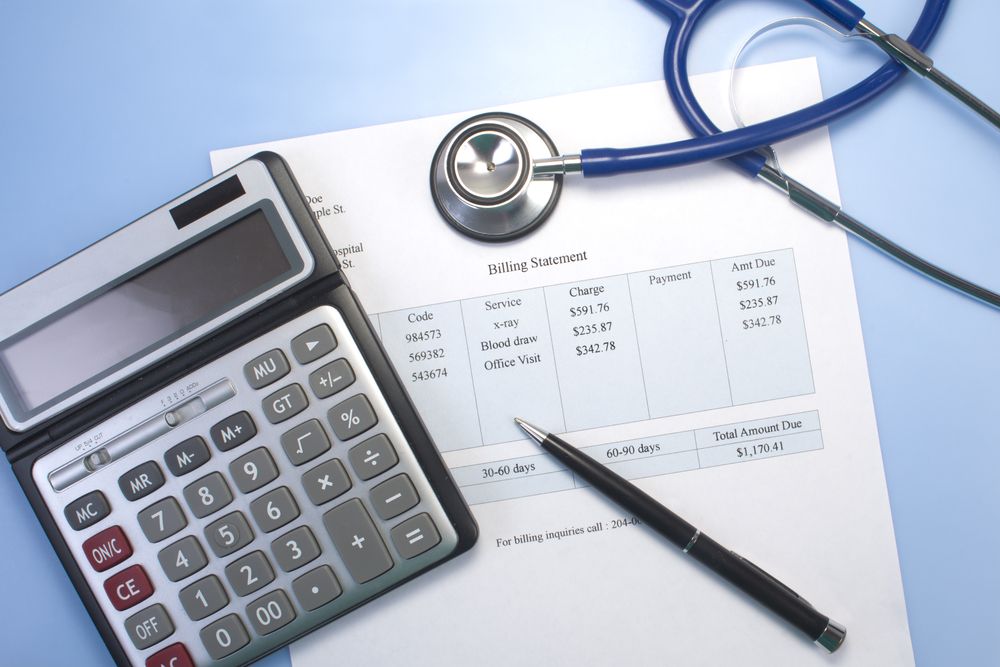
Inaccurate coding is a common challenge in healthcare that can lead to denied claims, compliance risks, and financial losses. Medical auditing services play a vital role in identifying and correcting these coding errors, ensuring that healthcare providers receive accurate reimbursement while maintaining compliance with federal and state regulations. By collaborating with specialized medical billing companies in the US, healthcare practices can improve their billing accuracy and reduce coding-related issues, leading to a more efficient revenue cycle.
What Are Medical Auditing Services?
Medical auditing services involve the systematic review of a healthcare provider’s coding, billing, and documentation processes to ensure accuracy, compliance, and efficiency. These services focus on evaluating how medical codes are assigned for various procedures, treatments, and diagnoses to ensure they align with federal regulations like HIPAA and CMS guidelines.
Core Components of a Medical Audit
Code Accuracy Verification: Checking whether the correct codes have been assigned to procedures and diagnoses.
Billing Process Review: Ensuring that all billed services are appropriately documented.
Regulatory Compliance: Verifying adherence to federal regulations, including HIPAA and Medicare/Medicaid rules.
How Do Medical Auditing Services Identify Coding Errors?
Medical auditing services deploy systematic processes to uncover coding inaccuracies that might otherwise go undetected. From reviewing patient records to verifying procedure codes, medical auditors conduct a detailed examination of coding practices within healthcare facilities. Working closely with medical billing companies in US, these services identify errors that could hinder revenue flow or result in compliance risks.
Reviewing Patient Records and Documentation

A core aspect of identifying coding errors is reviewing patient records to ensure documentation aligns with billed codes. Auditors check that all procedures listed in patient records have matching codes and that these codes accurately reflect the services provided. This review helps catch instances where a service might be billed at a higher rate than appropriate (upcoding) or where key services are omitted (under-coding).
Common Documentation Errors in Coding
Incomplete Patient Notes: Missing information can lead to incorrect code assignments.
Mismatched Procedures and Diagnoses: The procedure code should directly relate to the documented diagnosis.
Lack of Specificity: Vague descriptions can result in misinterpretation and incorrect coding.
Validating ICD and CPT Code Accuracy
To ensure compliance and reimbursement, medical auditors assess the accuracy of ICD (International Classification of Diseases) and CPT (Current Procedural Terminology) codes used in billing. They ensure these codes match the descriptions in patient records and are applied according to the latest regulatory standards.
ICD Codes: Used for diagnosis coding, ICD codes need to accurately reflect the patient’s condition.
CPT Codes: Common in billing procedures, CPT codes should represent the services provided as precisely as possible.
Medical auditing services monitor updates to these coding systems, ensuring that healthcare providers use the latest codes for their claims. Medical billing companies in the US often help providers keep up with these changes, reducing the chance of errors.
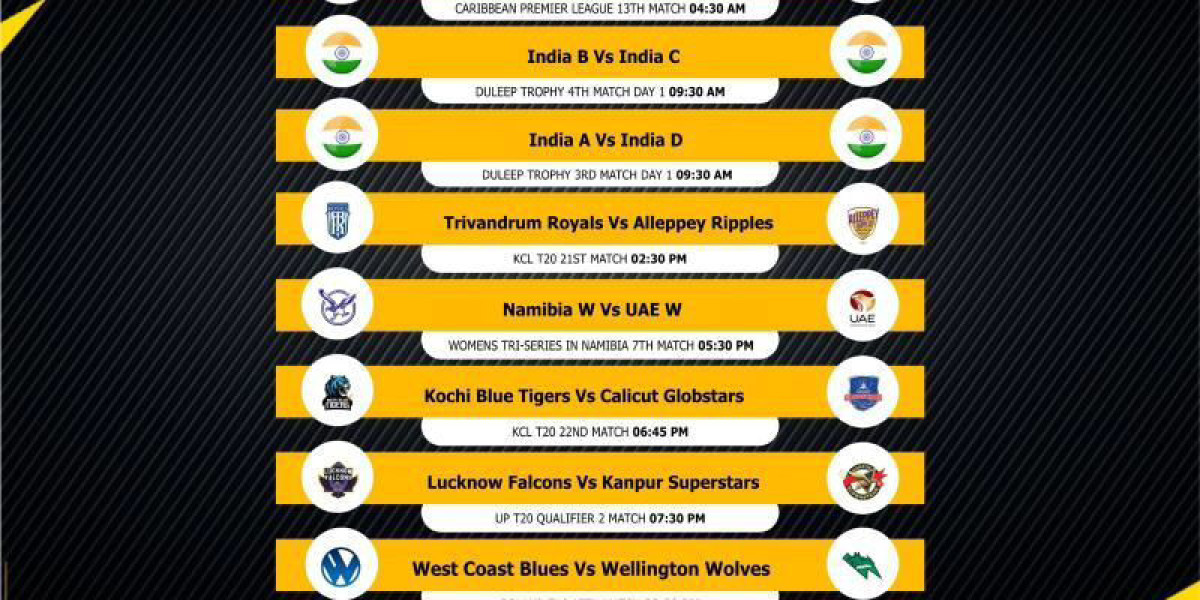
Common Types of Coding Errors Detected in Audits
Auditors frequently encounter certain types of coding errors in healthcare settings. Each of these errors can impact billing accuracy, revenue, and compliance, making it essential to identify and address them promptly.
Upcoding and Downcoding
Upcoding: Occurs when a healthcare provider assigns a higher-level code to a procedure or diagnosis than is warranted, leading to overbilling.
Downcoding: Assigning a code that reflects a lower level of service than provided, which results in lost revenue.
Auditors identify these errors by comparing the documentation in patient records with the codes assigned to each procedure. By correcting these discrepancies, medical auditing services prevent overbilling and underbilling, which can have financial and legal repercussions.
Misuse of Modifier Codes
Modifier codes are essential for indicating when a procedure or service has been altered in some way. However, improper use of these codes can lead to errors in billing. Medical auditors review the use of modifier codes, ensuring they accurately reflect the nature of each service.
Common Errors with Modifier Codes: Incorrectly applied modifiers can lead to payment denials or reimbursement delays. Auditors verify that each modifier accurately describes any special circumstances surrounding the procedure.
Unbundling Errors
Unbundling involves billing individual services separately when they should be bundled under a single code. This can result in higher charges and may violate insurance company rules. Medical auditing services detect unbundling by reviewing documentation to ensure codes reflect bundled services correctly, in compliance with payer guidelines.
How Medical Auditing Services Correct Coding Errors
Once coding errors are identified, medical auditing services provide corrective measures to help healthcare providers enhance their billing practices. By collaborating with medical billing companies in the US, auditors recommend and implement steps to correct these errors and improve long-term accuracy.
Conducting Training Sessions for Coding Staff

A common reason for coding errors is a lack of training among billing and coding staff. Medical auditing services often conduct training sessions to improve staff understanding of current coding standards and compliance regulations. This training helps prevent errors from recurring, ensuring the staff has the knowledge needed to apply the correct codes to each procedure and diagnosis.
Topics Covered in Training
Regulatory Updates: New or revised coding guidelines that impact billing processes.
Common Error Identification: Techniques for recognizing and avoiding typical coding mistakes.
Specificity in Coding: Emphasis on accurately documenting services to support precise coding.
Implementing Coding Software and Automation
Many medical billing companies in the US use advanced coding software and automation tools to improve accuracy. Medical auditors may recommend and help implement such tools within a healthcare provider’s billing process. Automation reduces human error, enhances efficiency, and ensures that coding practices align with the latest standards.
Coding Assistance Tools: Assist staff in selecting accurate codes based on the patient’s diagnosis and procedures.
Error Detection Algorithms: Software that flags potential coding discrepancies before claims are submitted.
Establishing Regular Internal Audits
For ongoing improvement, medical auditors recommend regular internal audits. These self-audits, conducted by the healthcare provider’s own team, help identify emerging issues before they become larger problems. By regularly reviewing coding and billing practices, providers can ensure compliance and keep their processes in line with current regulations.
Benefits of Internal Audits
Early Error Detection: Identify coding mistakes before claims are processed.
Continuous Process Improvement: Regular audits promote a culture of accuracy and diligence.
Reduced Claim Denials: Ensures that claims are accurate and complete, reducing the likelihood of denials.
The Role of Medical Billing Companies in Supporting Accurate Coding
Medical billing companies in the US are integral partners in helping healthcare providers maintain accurate and compliant billing practices. These companies specialize in both billing and auditing services, offering healthcare practices access to a wealth of expertise and resources. By working with a medical billing company, providers can streamline their billing processes, reduce errors, and ensure that they receive appropriate reimbursement.
Access to Expert Auditors
Billing companies often employ experienced auditors who understand the complexities of medical coding and billing. These professionals provide insights into best practices, staying up-to-date with the latest industry standards and regulatory changes. Their expertise can help healthcare providers correct coding errors quickly and efficiently.
Tailored Auditing Solutions
Medical billing companies offer customized auditing services that fit the specific needs of healthcare providers. These tailored services include everything from initial audits to full-scale compliance reviews, ensuring that providers have the support they need to maintain accurate and compliant billing practices.
Conclusion
Medical auditing services play a critical role in identifying and correcting coding errors, which can have far-reaching impacts on a healthcare provider’s revenue and compliance. By working closely with medical billing companies in the US, providers gain access to resources and expertise that help reduce coding errors, improve reimbursement, and ensure compliance with industry standards. Through comprehensive audits, training programs, and the implementation of automated tools, medical auditing services provide a framework for accuracy and efficiency in billing. For healthcare providers, investing in these services ensures a streamlined revenue cycle, minimizes compliance risks, and contributes to a more effective and reliable healthcare billing system.